Cerebral ischemia occurs when there isn’t sufficient blood flow to the brain to meet its metabolic needs.
Usually, it occurs as a result of either global cerebral hypoperfusion or a vascular territory lack of blood supply (stroke).
There are 2 types of strokes: ischemic (a blood clot blocking an artery) and hemorrhagic (an artery rupture that results in bleeding (see link for hemorrhage).
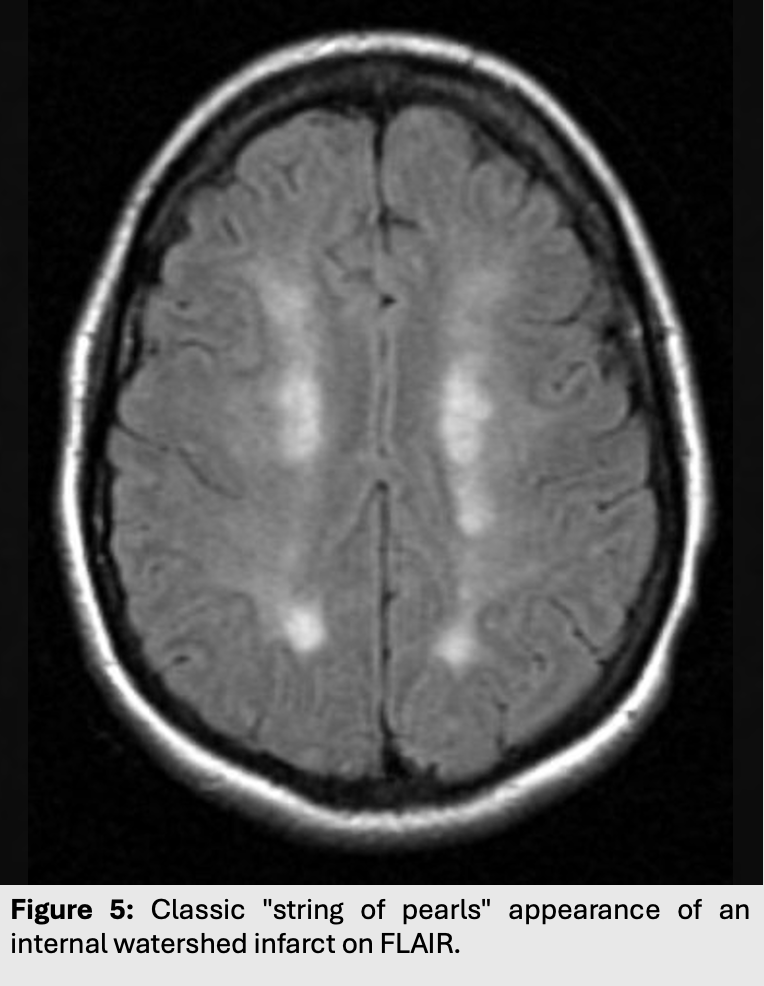
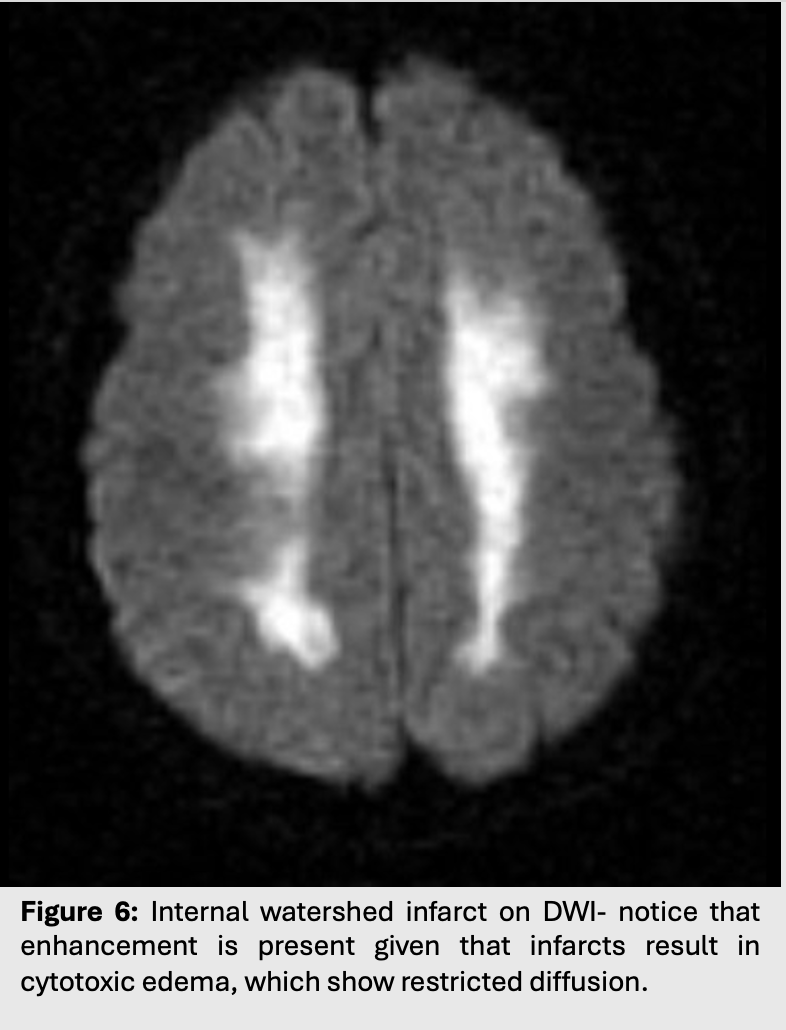
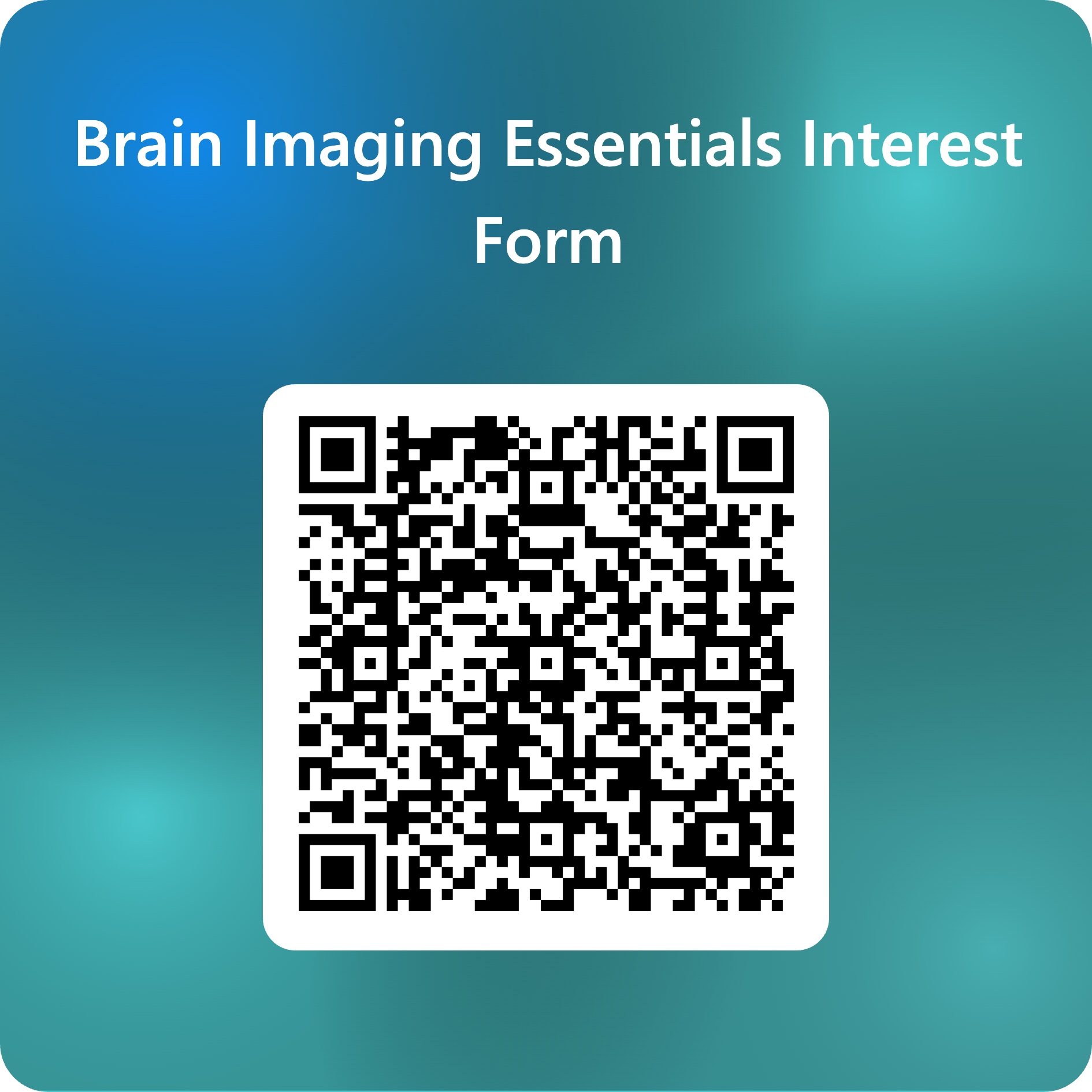
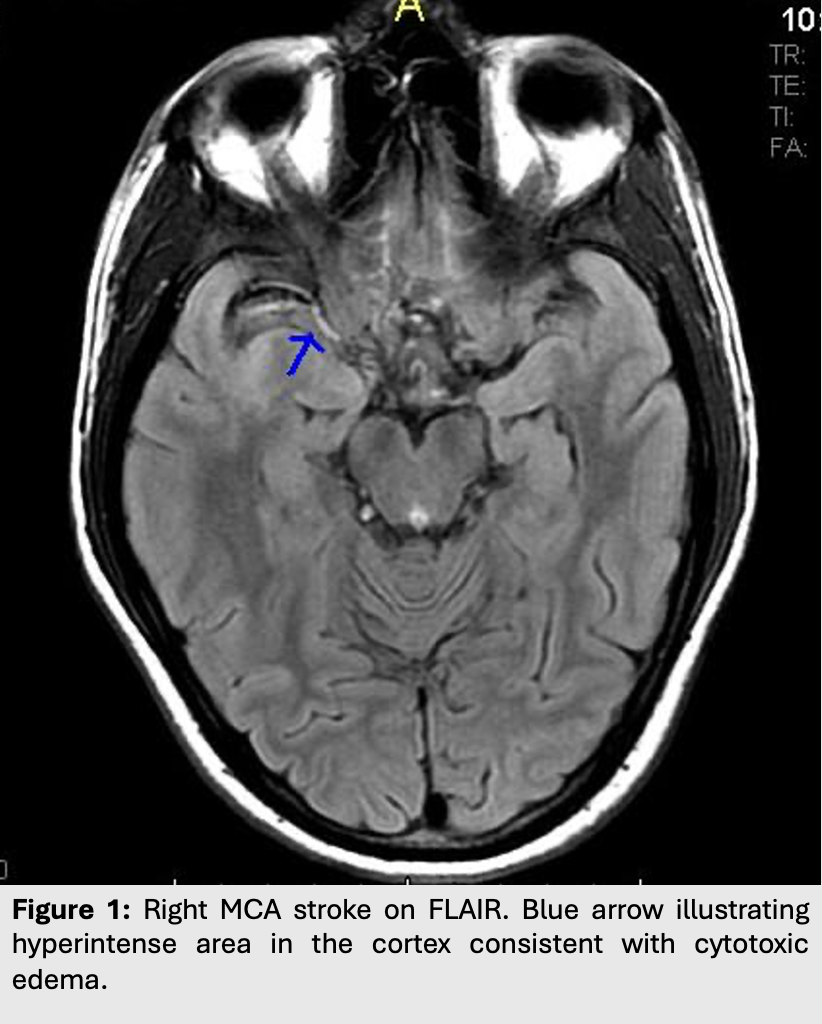
In general, ischemia causes cytotoxic cerebral edema which can be best evaluated with a combination of T2 and DWI.
If the infarct is located near the ventricles or the cortex, FLAIR (dark CSF) may be favoured over T2 (hyperintense CSF), because it allows better contrast between CSF and the lesion.
- Ischemic stroke
- Ischemic strokes make up around 90% of all strokes and are usually caused by sudden vascular occlusions secondary to thromboemboli.
- Patients suffering from ischemic stroke usually present with focal neurological deficits.
- Initial workup involves a non-contrast CT of the head—which could look completely normal if the infarct is less than 3 hours old! Followed immediately by a CTA to assess the vessels.
- Clinical tidbit: The purpose of the initial non-contrast CT is to rule out hemorrhage, which will guide management by allowing doctors to prescribe thrombolytic therapy.
- In acute ischemic strokes, changes on imaging usually take time to appear.
- Although MRI is not the imaging modality of choice for acute stroke in most Canadian centers (lack of availability and longer time to scan), it can rapidly and accurately characterize the infarct.
- Cortical edema takes at least 3 hours before it can be seen on T2/FLAIR (hyperintense with cortical thickening and loss of grey-white junction differentiation).
- However, it only takes between 10 to 60 minutes for and acute MCA infarct to be seen on DWI.
- Global cerebral hypoperfusion
- Global cerebral hypoperfusion occurs when there is an overall decrease in cerebral perfusion, which can result from systemic causes such as hypotension and shock or it can be a result of increased intracranial pressure (increased ICP decreases cerebral perfusion pressure).
- Often times, systemic causes of hypoperfusion are worsened by severe stenosis or atherosclerotic occlusion of the carotid or major cerebral arteries to cause ischemia.
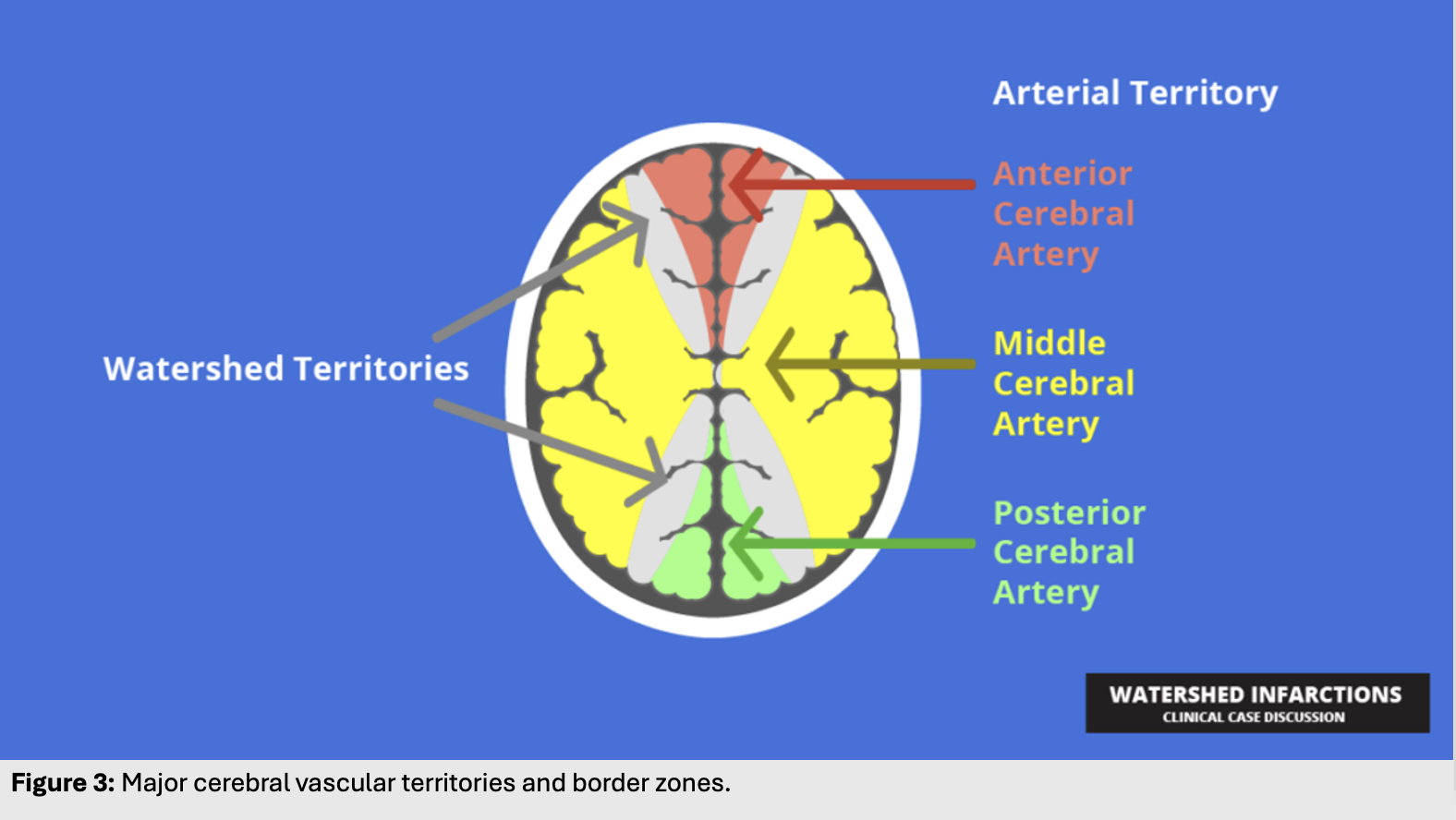
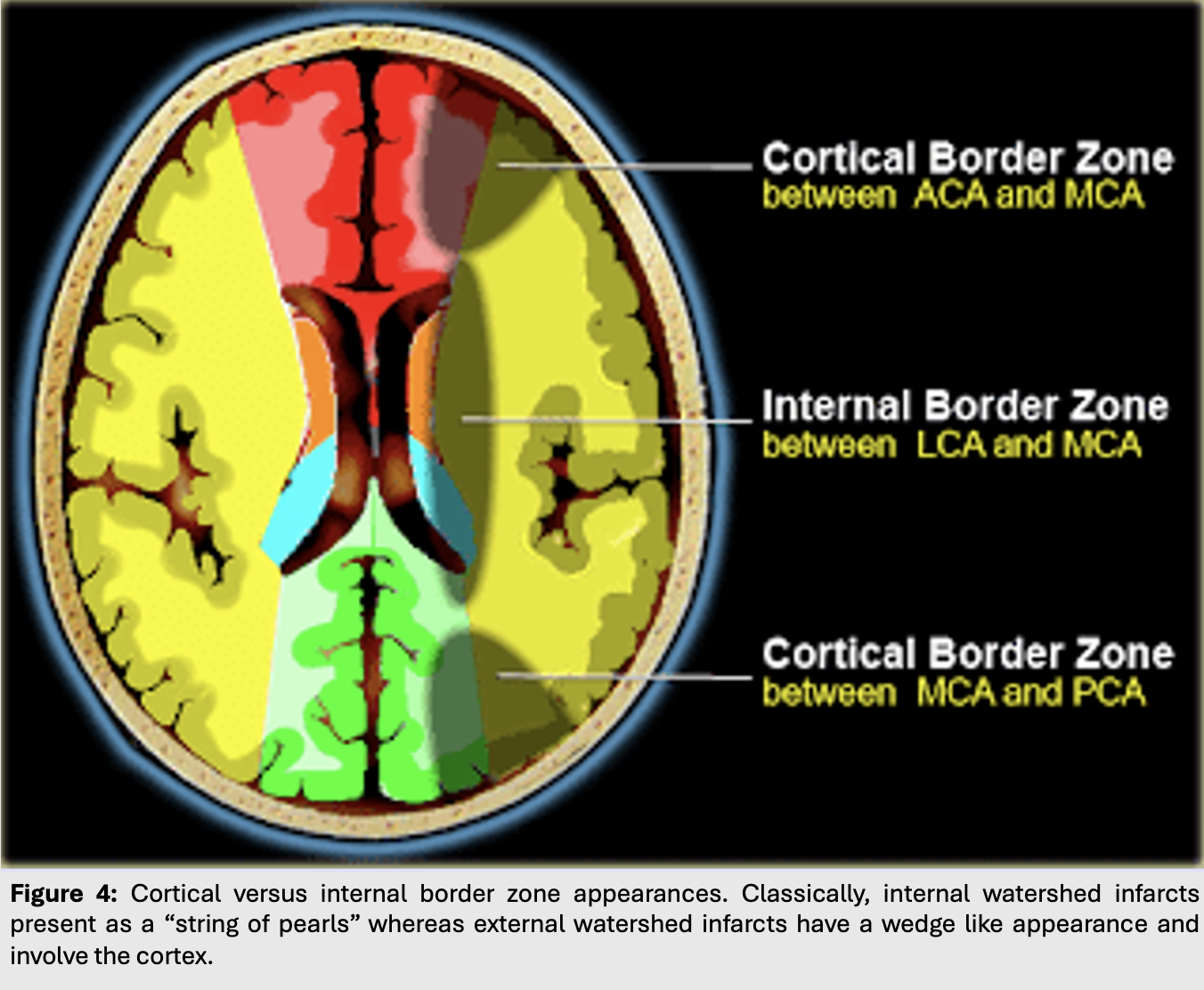
- In these scenarios, the first areas of the brain to suffer from ischemia will be those furthest away from major arteries.
- Infarcts of this kind are called watershed or border zone infarcts as they happen on the borders of major vascular territories.