Disorders of abnormal myelination fall under the realm of white matter disorders. Most frequently, we talk about demyelinating diseases, which are when there is a loss of normal myelin around axons in the CNS. However, abnormal myelination also includes dysmyelinating disorders, which are characterized by structural or functional defects of the myelin sheath, or hypomyelinating disorders, when there is a lack of normal myelin.
Leukodystrophy is a term that is often used interchangeably with ‘white matter disorder’; although it has no precise, agreed-upon definition, leukodystrophies tend to be white matter diseases with a heritable component.
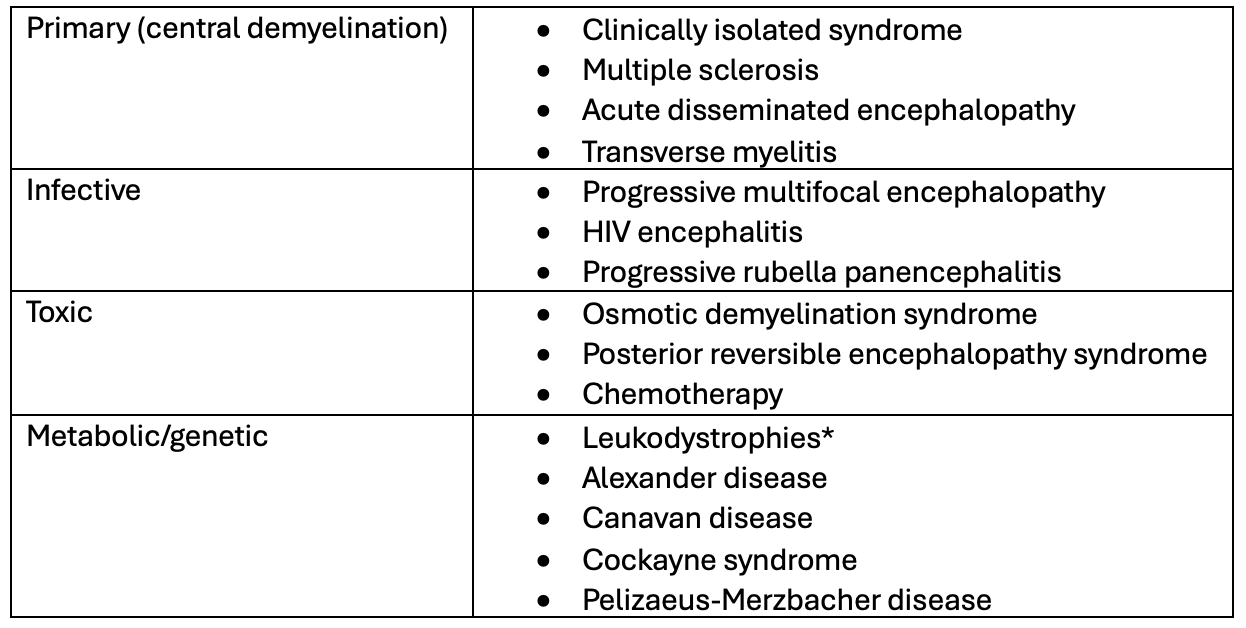
Table of demyelinating diseases
The Demyelinating Protocol is used to determine what MRI sequences and why to use when diagnosing and/or following demyelinating diseases.
When attempting to make a new diagnosis, the following sequences are used:
- T1
- Named the anatomical sequence, T1 best allows us to assess parameters of normal brain anatomy.
- For instance, volume loss is important to search for in cases of suspected Multiple Sclerosis (MS) as it is correlated with disease severity and disability.
- White matter lesions typically look hypointense compared to the surrounding healthy white matter (rich in lipids).
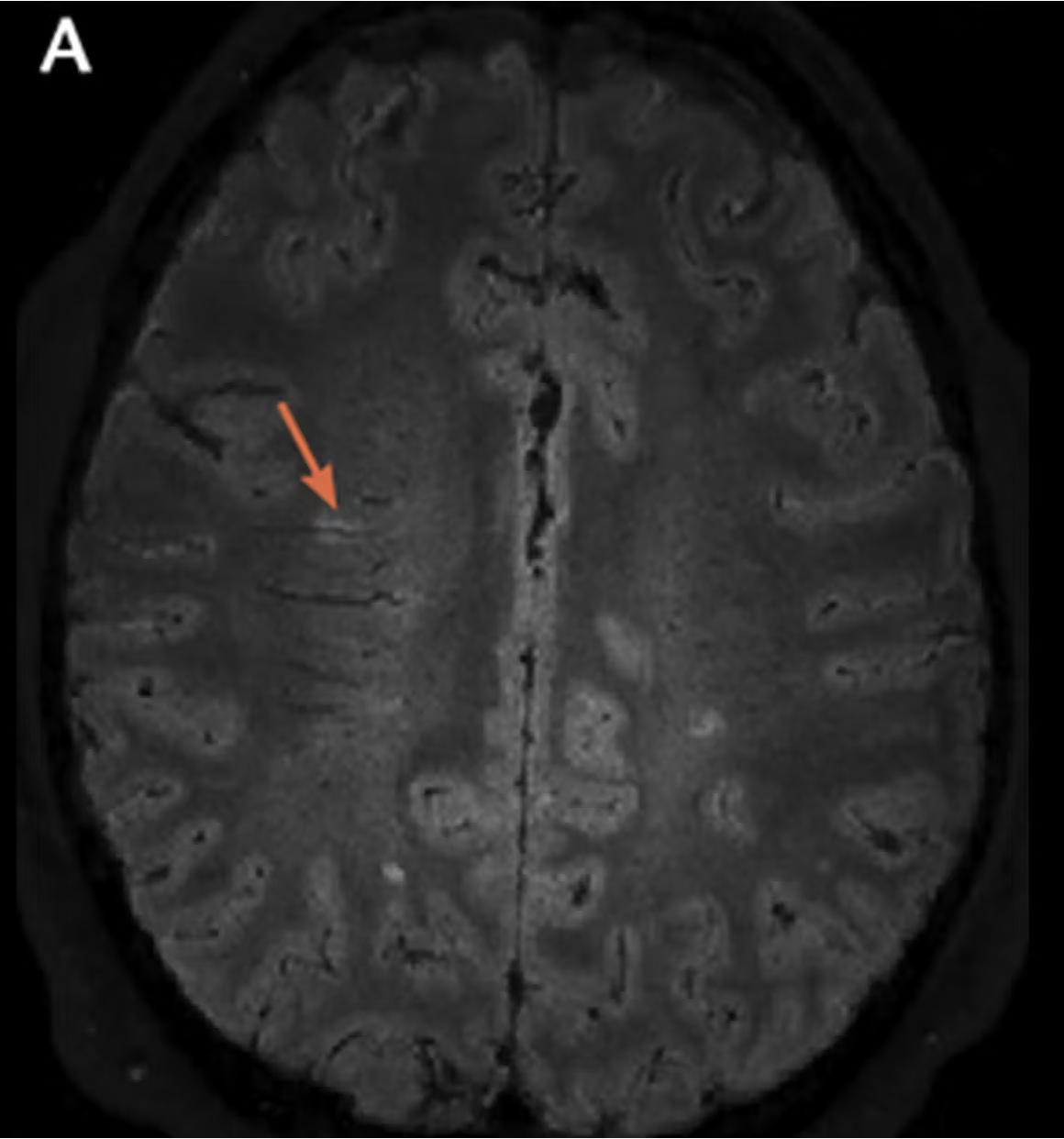
- T2 & FLAIR
- These two sequences give the best view of white matter lesions which appear hyperintense due to the edema resulting from glial cell injury.
- Both active and old white matter lesions will appear as hyperintensities on T2 and FLAIR.
- FLAIR is usually preferable to T2 for supratentorial lesions (above the tentorium cerebri) as it eliminates distracting signal from the ventricles but T2 is superior for infratentorial lesions.
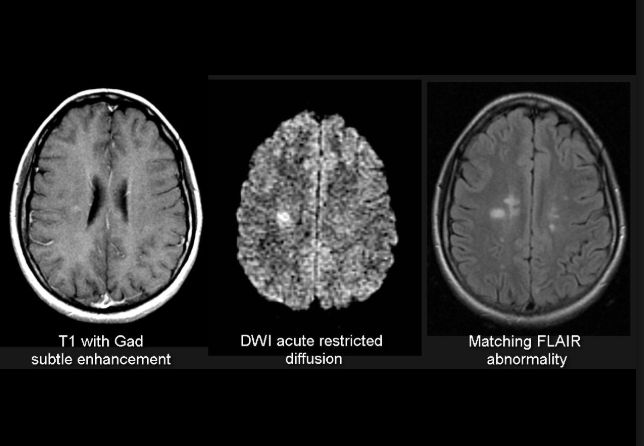
- DWI/ADC
- This sequence is used to look for active demyelinating plaques, which may show restricted diffusion.
- TW C+
- Contrast is used to look for active demyelinating lesions.
- The active state of inflammation leads to a disruption in the BBB that allows contrast to pass through, resulting in an open ring enhancement pattern.
For follow-up imaging, the same sequences are used minus the contrast, unless there is concern for rapid disease progression.
Different demyelinating disease distinguish themselves from the pattern and distribution of the white matter lesions through the CNS, as well as clinical history, symptoms on presentation and genetic patterns.
For instance, MS lesions are typically round or ovoid in shape and should generally be >3mm from their long axis.
They are usually located in the periventricular, juxtacortical/cortical and infratentorial regions as well as the spinal cord. If you want to know more about MS on imaging, this is a great resource.
Here are some examples of typical multiple sclerosis lesions:
Distinguishing between the imaging patterns of demyelinating diseases takes many years of practice and experience, so we will not attempt to broach the topic now!
However, for those that are interested, we invite you to take a look into the Revised McDonald criteria for Multiple Sclerosis diagnosis or the following resource which broadly details the characteristics of different types of white matter lesions.